PROBIOTICS, FERTILITY, AND PREGNANCY
May 10, 2018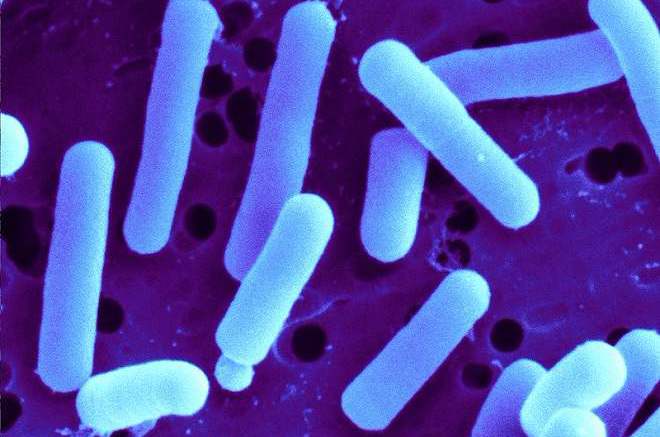
In addition to the work I LOVE talking with clients and helping to educate couples on infertility and how they can address is naturally, I also do a LOT of professional writing, for journals whose aim it is to guide research and guide clinical practice of other doctors. This article, originally published in Natural Medicine Journal, is a summary of a study that was published in 2012- I add interpretation about how it should influence a doctor's clinical practice.
Interestingly, this is STILL such an interesting topic that I was invited to speak (and did speak) at the NH Osteopathic Medical Society conference earlier this year on this same topic! That's right, the conventional medical doctors are starting to pay attention to probiotics! It was such a basic talk, as it was really an introduction to new material for this audience, but I'm SO SO glad that they wanted to dive in!
Now, with fertility and healthy pregnancy, more and more info has been published demonstrating the importance of the right flora (or probiotic bacteria) in the vaginal vault for general vaginal health, for fertility & a healthy pregnancy, and most of the research has been on the health of the babies!
If you don't pay attention to your vaginal flora now, it's time! Read on! And if you want my commentary on how this impacts different aspects of fertility, I'd suggest you join the Perfect Fertility family and sign up to receive my weekly dose of fertility & love in your inbox... I save the juiciest stuff for my email list VIPs!!
Without further ado... here it is!
STUDY INVESTIGATES THE IMPACT OF PROBIOTICS ON PREGNANCY PROGRESSION
REFERENCE
Stojanovic N, Plecas D, Plesinac S. Normal vaginal flora, disorders, and applications of probiotics in pregnancy. Arch Gynecol Obstet. 2012;286:325-332.
DESIGN
Observational, randomized, prospective study.
PARTICIPANTS
Eligible women (N=60) between 18 and 45 years of age and between 16 and 22 weeks gestation at time of enrollment were systemically randomized to either the active (n=30) or untreated (n=30) (control) group.
STUDY PARAMETERS
The intervention group received vaginal insertion of Lactobacillus rhamnosus BMX 54 (40 mg containing 40,000 colony forming units), 1 per week for 12 weeks (n=30). Every 4 weeks, vaginal and cervical swabs were collected and pH, quantity, and quality of vaginal discharge were measured. Additionally, the consistency, length, and dilation of the cervix was measured, as well as the level of the presenting part of the fetus relative to intraspinous diameter.
KEY FINDINGS
In untreated women, there was an increase in pathogenic microorganisms found in the vaginal and cervical swabs (P<0.05) as well as an increase in average pH values (P<0.05), the amount of vaginal discharge (P<0.05), and a positive “whiff test” (P<0.05) over a 12-week time period. Additionally, a significant trend was also observed for a decrease in the length of the cervix (P<0.0001), an increase in dilation of the cervix (P<0.05), and a lower position of the fetus (P<0.0001). In the treatment group, there was a significant decrease in the cervical length at the final timepoint (P<0.01), but no other changes noted in the other measurements.
In the untreated women, the number of woman with pathogenic organisms measured on vaginal and cervical swabs increased over the treatment time. At the study onset, 11 women in the control group had altered vaginal and cervical flora (detected pathogens included C. albicans, E. coli, Enterococcus, Streptococcus beta-haemolyticus, Proteus mirabilis, Staphylococcus, and Chlamydia trachomatis). At the 4-week mark, the number of women with altered flora was 18, a statistically significant increase (P=0.0410). Among the treatment group, 11 women began the study with altered flora and at the end of the study, only 1 woman had altered vaginal and cervical flora (a nonsignificant change, P=0.1630).
Overall, all parameters measured come together to demonstrate that the presence of abnormal vaginal flora negatively influenced several parameters that are indicative of healthy progression of pregnancy, and that the treatment of women with vaginal application of Lactobacillus rhamnosus BMX 54 during pregnancy was effective in preventing the alteration of those parameters.
PRACTICE IMPLICATIONS
Vaginal application of probiotics has previously been observed as effective in preventing the development of vaginal infection in the normal population.1 This study first confirms the importance of healthy vaginal ecology on parameters that are commonly associated with healthy progression of pregnancy.
It has also been previously demonstrated that the presence of bacterial vaginosis or aerobic vaginitis can be associated with adverse pregnancy outcomes, including an increased rate of miscarriage and increased preterm delivery.2,3 These outcomes can also occur in women with asymptomatic infection.4
IT WOULD BE PRUDENT TO SCREEN FOR VAGINAL INFECTION, AS EVEN ASYMPTOMATIC INFECTIONS MAY LEAD TO ADVERSE PREGNANCY OUTCOMES INCLUDING PRETERM BIRTH.
The mechanism by which these pathogenic flora impact cervical competence is not well understood. Regardless of the mechanism, it is clear that vaginal ecology has an effect on the ability of the cervix to maintain a pregnancy, and that administration of a vaginal suppository of Lactobacillus is effective to not only correct vaginal ecology, but in this case, to also mitigate the risk of preterm birth associated with the presence of pathogenic flora in the vaginal vault.
In conclusion, it would be clinically prudent to screen women for vaginal infection, as even asymptomatic infections may lead to adverse pregnancy outcomes including preterm birth. Vaginal administration with Lactobacillus rhamnosus BMX 54 should be considered for women with altered vaginal ecology and considered in women at risk of vaginal infection.
LIMITATIONS
This study was small, and there was a nonsignificant difference in the number of women observed to have pathogenic microorganisms in their vagina at the onset of the study between the control and study groups.
Also of note was that in this study, when a woman was diagnosed with a vaginal infection, she was treated with oral or vaginal administration of antimicrobial agents. When women were treated with antibiotics, this medication would certainly also have affected the woman’s Lactobacilli status, thus removing the innate protection that a healthy colonization of Lactobacilli supplies.
REFERENCES
1. Ehrstrom S, Daroczy K, Rylander E, et al. Microb Infect. 2010;12:691-699.
2. Marcone V, Rocca G, Lichtner M, et al. Int J Gynecol Obstet. 2010; 110:223-226.
3. Donati L, Di Vico A, Nucci M, et al. Arch Gynecol Obstet. 2010;281(4):589-600.
4. Leitich H, Kiss H. Best Pract Res Clin Obstet Gynecol. 2007;21(3):375-390.







